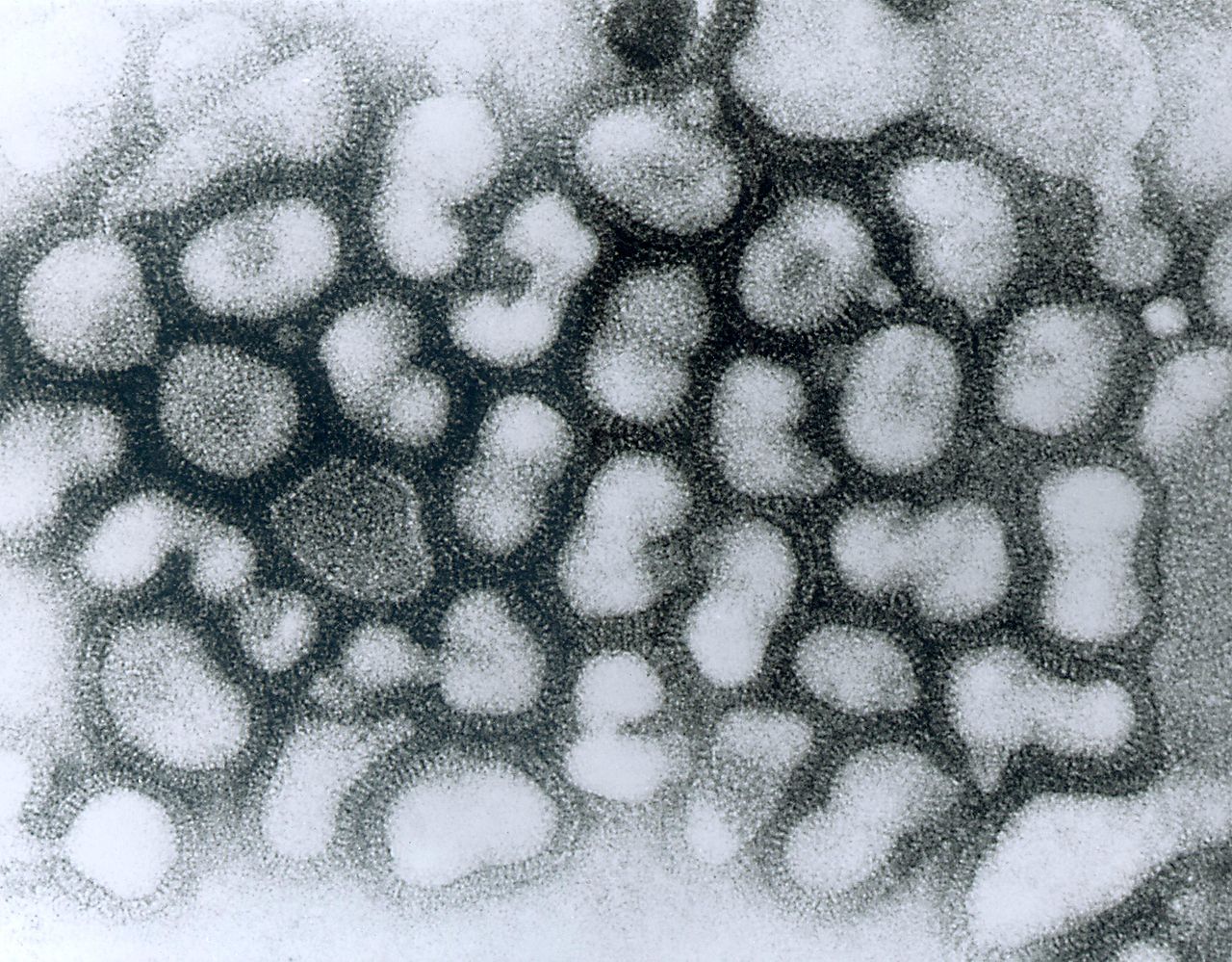
Transmission electron micrograph of the influenza A virus. Image courtesy of Centers for Disease Control and Prevention.
by Benjamin Recchie
Influenza is a tricky disease to fight because it evolves rapidly, which means that the vaccine that protects you today might not be as effective a few years later as new strains of the virus appear. Strangely, these new strains of flu seem to pop up from one part of the world—a heavily populated swath from India through Southeast Asia and China—then make their way across the globe. Understanding how this happens is no academic exercise: the influenza subtype H3N2 kills an estimated 250,000 to 500,000 people each year worldwide. UChicago researchers Sarah Cobey, assistant professor of ecology and evolution, and second-year graduate student Frank Wen decided to take a crack at solving this puzzle by modeling the spread of H3N2.
A common explanation of the prevalence of Asian strains of flu is seasonality. In temperate areas, there is a defined flu season, but in the tropics flu appears year round. Since most of East and Southeast Asia’s population lives in a tropical or subtropical environment (the theory goes), flu might thrive and evolve faster there than in temperate areas, where influenza infections “shut down” for several months. There are other hypotheses, too. One is sheer population size (East, South, and Southeast Asia house roughly half the world’s people), which provides more bodies for flu to evolve in; another is the high rate of population growth in that region, which provides new people for the virus to infect. Then there’s the fact that the H3N2 virus first appeared in Hong Kong, which means it’s had longer to evolve there than anywhere else; and finally there’s the hypothesis that higher transmission rates in that part of the world allow new strains to spread faster there than anywhere else.
Wen and Cobey adapted a model by a collaborator (Trevor Bedford, at the Fred Hutchinson Cancer Research Center) to represent the dynamics of influenza in a population representing the temperate northern and southern hemispheres and the tropics. Since this model used much more memory than any of their lab’s own computers could provide, explains Wen, they turned to the RCC’s high-performance computing cluster, Midway. They then ran Monte Carlo simulations, testing thousands of iterations of their model under different conditions.
What they found surprised them: the key parameter turned out not to be seasonality after all, but rather transmission rates. “Populations with slightly higher transmission rates would produce strains that have a transmissive advantage and are more likely to spread globally,” says Wen. “In reality, transmission rates are difficult to measure, so using a computational model was essential to understanding the observed patterns.”
Cobey explains where the researchers are going next: “We're interested in seeing how vaccination affects the phylogeography of flu, and we're doing this first by simulation (right now in just one population!) and will then look to see if flu evolution in different regions is affected by vaccination rates,” she says. If, for example, they find that a coordinated vaccination campaign in East and Southeast Asia might hobble flu viruses there before they can spread, that could lead to a major breakthrough for public health. And given that influenza kills hundreds of people daily, every new tool in the hands of health authorities means lives saved.